Proximal Humerus Fractures
Background
The shoulder joint is a complex structure, referred to as a ball in socket joint, composed of the proximal (upper end) of the humerus and the glenoid cup of the scapula. The main advantage of the shoulder is the wide range of motion it provides. Within and surrounding the joint are multiple ligaments, tendons and cartilaginous structures that provide smooth motion and stability. In order to function appropriately, the humeral head and glenoid must have a smooth surface and the humeral head must be centered appropriately in the glenoid throughout range of motion. If this proper anatomy is disrupted, dysfunction may occur acutely or over time.

Proximal humerus fractures
Although multiple fracture patterns may occur with trauma, we will focus on proximal humerus fractures given these fractures are the most common fractures in the shoulder. These fractures usually occur in the elderly from a fall but certainly can happen in all age ranges with higher energy trauma.
Most proximal humerus fractures can be treated non-operatively. This is because the proximal humerus has robust vascularity and most fractures maintain good bony contact amongst the main fracture fragments allowing for adequate bone bridging and healing without surgical intervention. There are several things to consider when deciding to perform surgery or not. Decision points for surgery include neurovascular compromise, amount of displacement, joint surface involvement/displacement, tuberosity involvement, underlying health of the joint and overall health and activity level of the patient.
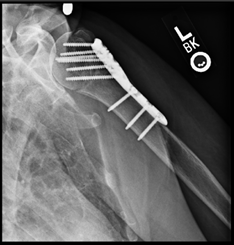
If surgery is determined the best approach, options include pinning, screw fixation, plating with screws, rod placement or even a shoulder replacement. Risks include non-union, infection, hardware failure or neurovascular injury.
Rehabilitation
For both surgical and non-surgical management, the patient will be placed into a sling for 2-4 weeks with no mobility of the shoulder to allow some healing of the fracture. The patient may move the elbow, wrist and hand during this time. The patient will then initiate occupational/physical therapy to minimize shoulder stiffness. When to start therapy and how fast to progress rehabilitation is made on a case by case basis depending on the stability of the fracture and the rate of healing. The orthopedic team will obtain xrays over the next several weeks to monitor for healing of the fracture and help guide rehab progress.
Wound Care
If surgery is performed, you will be placed in a long arm splint and or a sling to protect the fracture and the wound. The wound is often dressed with a waterproof Aquacel dressing and will remain in place until your first postoperative visit. This dressing can get wet in the shower but do not soak the dressing or wound in tubs/pools. If standard dressings are applied, these will be removed 48-72 hrs after surgery. On postop day 5, the wound can get wet in the shower but no tubs or pools. Tubs and pools (submerging the wound) is avoided for usually 4 wks. If there are any concerns with the wound, please don’t hesitation to call the orthopedic team or present to the ER.