Cubital tunnel syndrome (CuTS) is the second most common nerve entrapment syndrome (second to carpal tunnel syndrome). This compression neuropathy involves the ulnar nerve as it courses through the cubital tunnel on the inside of the elbow. The cubital tunnel is formed by a groove between the medial epicondyle and olecranon of the elbow which is spanned by the cubital tunnel retinaculum. Primary functions of the ulnar nerve includes innervation of the hand providing both sensory and motor function, although there is some function, albeit less applicable to this topic, in the forearm. For purposes of this topic, we will focus on the effects of CuTS in the hand.
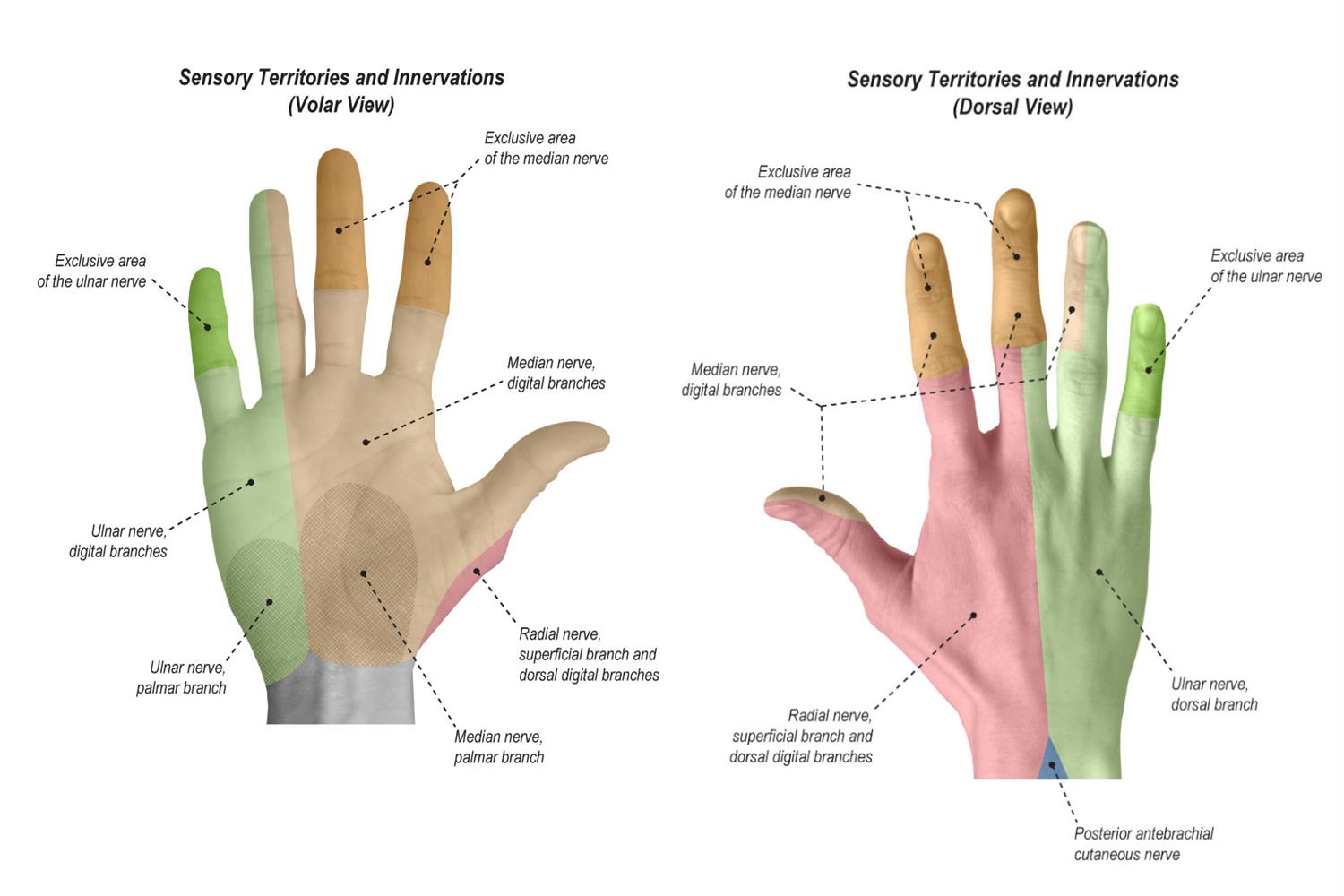
The ulnar nerve provides sensory function to the dorsal and volar aspect of the little finger and medial portions of the ring finger and hand. Motor function involves the interossei muscles (spreads and pulls fingers together), hypothenar muscles (controls little finger on the palmar side), adductor pollicus (brings thumb to hand), lumbricals (flex MCP joints and extend IP joints such as during the upstroke of writing) and deep head of the flexor pollicus brevis (flexes thumb).
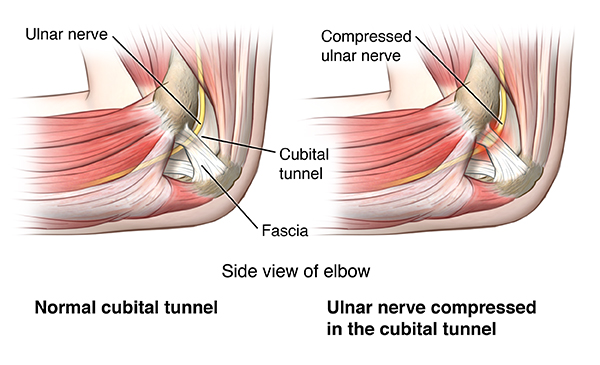
Given the involvement of the ulnar nerve to the ulnar side of the hand, patients with CuTS will often feel their hand go numb or "fall asleep" in the little and ring finger. This is often associated with the elbow being in a bent/flexed position. The elbow flexed position puts tension on the ulnar nerve as this compresses the cubital tunnel. Extension of the elbow relaxes the cubital tunnel, thus, releasing pressure on the nerve in some people. Thus, some patients will want to shake their hand when it goes numb in an effort to "increase circulation" to the hand. However, the more likely reason for the resolution of hand numbness when shaking the hand is the elbow being in a more extended position. Some patients' occupation put them at higher risk of CuTS due to their elbows being bent or constant pressure being placed on the ulnar nerve. In more severe cases of CuTS, there is a constant compression of the nerve causing constant symptoms of pain, numbness, and/or weakness in the hand. Over time, the muscles of the hand can cause permanent atrophy.
The clinic evaluation of patients with suspected CuTS includes a variety of tests to reproduce the symptoms. Your provider may also order a nerve conduction and electromyelogram (NCS/EMG) test to identify the location of nerve entrapment to help with confirmation of the diagnosis. It should be noted that cervical nerve entrapment may present similar to a CuTS and you may be asked to get an X-ray of the cervical spine at your visit. Once the diagnosis is confirmed with history, clinical evaluation and possibly an EMG/NCS, appropriate treatment options will be discussed based on severity and impact on life.
Non-operative treatment options include NSAIDs, activity modification, and night splinting to prevent flexion of the elbow (can wrap a towel around the elbow). Conservative treatment is effective in roughly 50% of patients.
If non-operative therapy fails or if symptoms and entrapment are more severe, then surgical intervention via a cubital tunnel release (CuTR) may provide the best outcome. This is an outpatient procedure which includes an incision along the medial aspect of the elbow and a release of the cubital tunnel retinaculum. In prolonged severe entrapment of the ulnar nerve, muscle wasting, weakness and numbness in the hand may be permanent. In these cases, surgery would be beneficial to halt the progression of symptoms even further. Once surgery is complete, the skin is then closed, a soft dressing placed, and the patient avoids elbow flexion passed 90 degrees for 2-4 weeks depending on wound healing.
After discharge from the hospital, the bandages are left in place for 48 hrs. In 72 hrs, the incision can get wet in the shower if there is no active drainage. We recommend no submerging of the wound for 3-4 wks. If drainage persists, the patient should notify their orthopedic team.
