Background
Hip arthroscopy is a minimally invasive hip preservation procedure. This procedure is quite technically demanding and requires additional training in order to perform. Dr. Lee specializes in hip arthroscopy and will be able to determine if you are an appropriate candidate for this procedure.
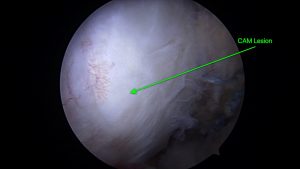
Hip arthroscopy is usually chosen for patients with acetabular labral tears or bony abnormalities within the hip joint. The labrum is a piece of cartilage that goes around the acetabulum (cup) of the hip. There are two common bony abnormalities which can cause labral tearing. These are a pincer deformity and a CAM lesion. If either of these two issues are present, the patient is at risk of a condition called femoral acetabular impingement (FAI), resulting in a labral tear. Often, a patient will have both a pincer and a CAM lesion.
Pincer deformities are bony over-hangings of the rim of the acetabulum. CAM lesions are benign bony formations of the femoral neck or head. If either condition is present, there can be pain in the groin with hip flexion. The pain is likely coming from impingement on the labrum.
After reviewing your X-rays and performing a physical exam, your provider may order an MRI with or without contrast to further assess the hip. We will be looking for cartilage quality, bony abnormalities and the quality of the labrum.
Treatment options for FAI/labral tears include NSAIDs, steroid injections, therapy to improve joint stability or surgery. The steroid injection can be performed under ultrasound guidance in our clinic and is tolerated quite well by patients.
If surgery is recommended, there are a few factors that are considered to determine if hip arthroscopy is appropriate for you. These considerations include but are not limited to: age, activity level, joint cartilage quality, medical history, etc.
If hip arthroscopy is elected for, there are a few procedures that are commonly chosen. These include resecting the pincer deformity, shaving down the CAM lesion, performing a labral repair or reconstructing the labrum. Sometimes, addressing pathology in a nearby tendon is performed arthroscopically but this is less common.
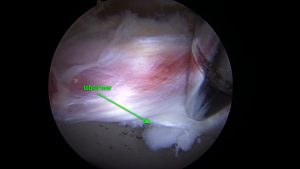
Labral Repair

This procedure includes implanting anchors into the acetabulum at the site of tearing and securing the labrum in an appropriate position to heal correctly.
Labral Reconstruction
If the labrum is too damaged to perform a repair, Dr. Lee may decide to reconstruct the entire labrum. In this procedure, the labrum is removed completely and a cadaver graft is introduced through the scope portals (incisions) and secured in place around the acetabulum with anchors and non-absorbable suture.