Background
A proximal hamstring injury (injury to the hamstring closest to the buttock) is a common sports related injury that often occurs during the eccentric phase of muscle contraction where the muscle begins contracting in an elongated position.
There are 3 big muscles in the hamstring (HS) called the semimembranosus, semitendinosus, and the biceps femoris. The attachment sites of these structures cross two joints, the hip and the knee.
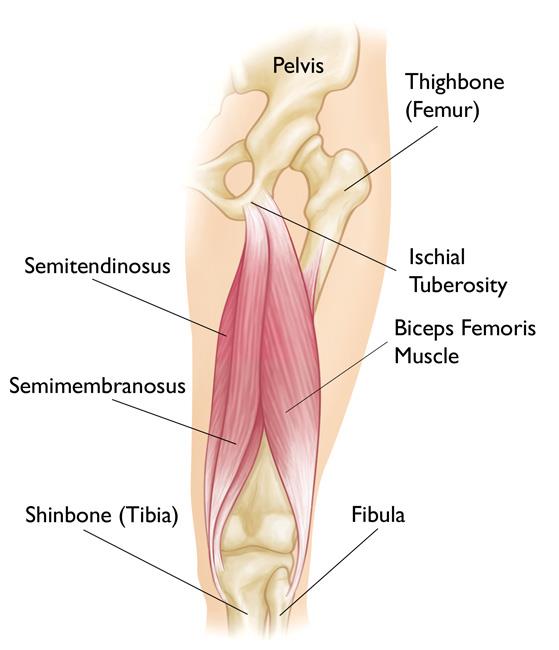
Therefore, they serve a dual purpose, to extend the hip and flex the knee. The HS structures are placed on highest stretch during hip flexion and knee extension. Thus, movements found in running, kicking sports and dancing (high kicks) place the HS at increased risk of injury.
Proximal Hamstring Injuries
Proximal hamstring injuries can be a significant source of pain and dysfunction. They can occur by participating in high level athletic or merely stumbling wrong and trying to catch yourself. Some patients will consider the injury minor and ignore the pain thinking it will resolve but notice lingering pain near the fold of the buttock. This can often be aggravated with sitting on hard surfaces. Gait disturbances are common in order to avoid knee flexion and hip extension. Certainly more significant injuries have a more significant pain presentation and patients often seek medical evaluation sooner. A bulge or even a mass or bruising from blood collection may be present.
Through a thorough examination, your orthopedic team will be able to help identify a hamstring injury. X-rays, and possibly an MRI, will be ordered to grade the level of injury.
Although there are several methods of grading proximal hamstring injuries, for the intent of this discussion we will classify them into 4 grades:

Treatment
Treatment of hamstring injuries is often conservative in nature and usually involve acute single tendon injuries or acute injuries with <2cm retraction. Chronic injuries can be treated conservatively even if more significant retraction or tendon involvement is present but not causing significant pain or dysfunction. Conservative modalities of care include:
Surgical Indications
Surgical considerations for repair of proximal hamstring injuries include but are not limited to:
It should be noted that surgery is most likely to be successful with less postoperative complications when conducted within 2 weeks of injury. This allows easier access to the injured tendon, facilitates mobilization of the tendon during fixation, prevents scarring of surrounding tissue and nerves, prevents progressive muscle atrophy and facilitates post-operative rehabilitation.