Hip Arthroscopy
Background
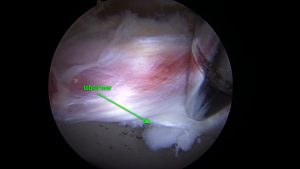
Labral Tear
Hip arthroscopy is a minimally invasive hip preservation procedure. This procedure is quite technically demanding and requires additional training in order to perform. Dr. Lee specializes in hip arthroscopy and will be able to determine if you are an appropriate candidate for this procedure.
Hip arthroscopy is usually chosen for patients with acetabular labral tears or bony abnormalities within the hip joint. The labrum is a piece of cartilage that goes around the acetabulum (cup) of the hip. There are two common bony abnormalities which can cause labral tearing. These are a pincer deformity and a CAM lesion. If either of these two issues are present, the patient is at risk of a condition called femoral acetabular impingement (FAI), resulting in a labral tear. Often, a patient will have both a pincer and a CAM lesion.
Pincer deformities are bony over-hangings of the rim of the acetabulum. CAM lesions are benign bony formations of the femoral neck or head. If either condition is present, there can be pain in the groin with hip flexion. The pain is likely coming from impingement on the labrum.
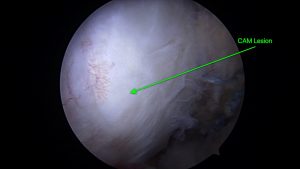
CAM Lesion
After reviewing your X-rays and performing a physical exam, your provider may order an MRI with or without contrast to further assess the hip. We will be looking for cartilage quality, bony abnormalities and the quality of the labrum.
Treatment options for FAI/labral tears include NSAIDs, steroid injections, therapy to improve joint stability or surgery. The steroid injection can be performed under ultrasound guidance in our clinic and is tolerated quite well by patients.
If surgery is recommended, there are a few factors that are considered to determine if hip arthroscopy is appropriate for you. These considerations include but are not limited to: age, activity level, joint cartilage quality, medical history, etc.
If hip arthroscopy is elected for, there are a few procedures that are commonly chosen. These include resecting the pincer deformity, shaving down the CAM lesion, performing a labral repair or reconstructing the labrum. Sometimes, addressing pathology in a nearby tendon is performed arthroscopically but this is less common.
Labral Repair

Labrum Repair
This procedure includes implanting anchors into the acetabulum at the site of tearing and securing the labrum in an appropriate position to heal correctly.
Labral Reconstruction
If the labrum is too damaged to perform a repair, Dr. Lee may decide to reconstruct the entire labrum. In this procedure, the labrum is removed completely and a cadaver graft is introduced through the scope portals (incisions) and secured in place around the acetabulum with anchors and non-absorbable suture.
Discharge and Rehab
Many patients stay overnight after this procedure but it is possible to go home the day of surgery. This will be discussed with Dr. Lee at the time of surgery.
The rehabilitation protocol for both labral repairs and reconstruction is the same. See below for our rehabilitation protocol. In addition, we will provide a “dot sheet” that you will take to your therapist to guide your rehab.
Postoperative Durable Medical Equipment Needs:
- Hip Brace – Bledsoe manufacturer
- Crutches
- Continous Passive Motion machine – start 0-60 degrees and increase 10 degrees per week
- Game Ready Hip or Thermotek Ice Machine x 3 weeks (optional)
- Hip abduction pillow between the legs x 3 weeks
- This must be worn at night or the hip must be in CPM overnight with towels laterally
- The need for a pillow is determined on a case by case basis
Postoperative Restrictions:
- 20% weight bearing x 3 weeks
- Full weight bearing at 4 weeks
- No ER past 10 degrees x 3 weeks
- No extension past 0 degrees x 3 weeks
- Avoid flexion with simultaneous internal rotation
Postoperative Prescription Medications:
- Voltaren 75 mg by mouth every 12 hrs x 14 days then Aspirin 325mg daily x 28 days
- Doxycycline 20 mg daily x 28 days
- Ondansetron 4mg by mouth every 8 hours as needed for nausea
- Cyclobenzaprine 10 mg by mouth every 8 hours as needed for spasm
- Oxycodone 5-10 mg by mouth q 4 hours as needed for pain
- Acetaminophen 1000 mg by mouth q 8 as needed for pain
- Docusate 100 mg by mouth every 12 hrs while on narcotics to prevent constipation
- Zolpidem 10mg by mouth at bed time as needed for insomnia
Postoperative Patient Management:
- Pain control
- ICE is extremely important factor
- Game ready (optional) when not in CPM
- IV and Oral pain medications
- ICE is extremely important factor
- Titrate down epidural and turn off by 2 hours postop
- Remove foley once epidural has resolved
- Start CPM immediately postop
- Range 0-60 degrees
- Avoid external rotation but nothing pushing on Common Peroneal Nerve
- First session should be 1 hour
- Expect drainage from the wounds the first day after surgery as fluid is mobilized out of the thigh. If persistent drainage (2-3 days), notify your surgical team.
- Range 0-60 degrees
Occupational Therapy Suggestions
- Pad handles on Crutches
- Cell phone always with you
- Get rid of rugs in the home to prevent falls
- Easy snacks
- Tegaderm to go home and place over incisions – so you can shower immediately postop
- CPM in one place so you don’t have to take it off the bed
- Wean off pain meds by day 3
- Antibacterial wipes – next to bathroom toilet to keep crutches clean
- Shower okay postop day 1
- One-hand Reacher for items on the floor