Rotator Cuff Tear
The shoulder has the greatest degree of motion of all joints in the body. It is a ball and socket joint in which the ball is the humeral head (proximal humerus) and the socket is a part of the scapula called the glenoid. However, because the glenoid is nearly flat the shoulder joint relies upon important soft tissue stabilizers one of which is the muscle and tendon complex called the rotator cuff. The rotator cuff has two functions; 1) position the humeral head near the center of the glenoid while stronger muscles such as the deltoid, pectoralis major, and latissimus dorsi move the arm, and 2) assist in movement of the shoulder such as reaching behind your back (internal rotation/subscapularis), reaching behind your head (external rotation/infraspinatus and teres minor), lifting your arm to your side (abduction/supraspinatus), and lifting your arm in front of you (forward flexion/supraspinatus). The rotator cuff is composed of four individual muscles whose tendons meld together to form a cuff of tissue that attaches to the top of the humerus. These fours muscles are the:
- Subscapularis
- Supraspinatus
- Infraspinatus
- Teres Minor
Additionally, there is a fluid filled sac called a bursa between the rotator cuff and the bone on top of your shoulder (acromion). The bursa allows the rotator cuff tendons to glide freely when you move your arm. When the rotator cuff tendons are injured or damaged, this bursa can also become inflamed and painful.
Rotator Cuff Tears:
A tear in the rotator cuff is a common cause of shoulder pain and disability among adults. Tearing the rotator cuff can cause pain, weaken your shoulder and limit the ability to move your arm. This can make many of the common things you do during the day painful and difficult to accomplish. Activities such as combing your hair, brushing your teeth, getting dressed and reaching overhead all require your rotator cuff.
Types of Rotator Cuff Tears:
A torn rotator cuff tendon is no longer fully attached to the humerus and depending on the extent of the tear, the muscle may not be able to fully move your upper arm. Most tears occur in the supraspinatus tendon and affect your ability to raise and rotate your arm. Sometimes other muscles are involved more commonly the infraspinatus or subscapularis. Over time, tendons may fray and as the damage progresses, may completely tear or at times one traumatic injury can cause a tear.
There are different types of tears.
- Partial Tears or partial-thickness tears, involve damage to the tendon, but do not completely separate the tendon from the bone. Partial tears are subdivided into tears that are on the joint side of tendon (articular sided tears) or on the top of the tendon (bursal sided tears).
- Full-Thickness Tear or a complete tear is a complete disruption of the tendon attachment to bone. Often tears occur where the tendons attach to the head of the humerus leaving a hole in the tendon.
Causes of Rotator Cuff Tears:
There are two main causes of rotator cuff tears: traumatic injury and degeneration.
Acute Tear
These are a result of an acute traumatic injury such as falling on an outstretched arm, or lifting something too heavy with a jerking motion which can tear the tendons that make up the rotator cuff. This type of rotator cuff injury may also occur with other shoulder injuries such as dislocations and broken collar bones
Degenerative Tear
Over your lifetime, the tendons slowly wear down. This is a natural part of the aging process and occurs more commonly in your dominant arm. A degenerative tear in one arm places you at higher risk for a tear in the other arm. Several factors contribute to degenerative, or chronic, rotator cuff tears.
- Repetitive motion stress. The same motions over and over can overtime result in overuse injury and tears in your rotator cuff. Sports with repetitive motions such as tennis and rowing can lead to wear of the rotator cuff. Even everyday household chores and activities can result in overuse injury and damage to the rotator cuff.
- Reduced blood supply. As we age, our circulation and ability to deliver blood to the rotator cuff tendons decreases and decreases the body’s natural ability to repair tendon damage ultimately resulting in tendon tear.
- Bone overgrowth, or bone spurs. Bone may develop on the underside of the acromion as we age, these bone spurs can rub on the rotator cuff tendons causing shoulder impingement. Over time, this constant rubbing will weaken the rotator cuff and make it more prone to tearing.
Risk Factors
Wear and tear with aging means that people over 40 are at greater risk of rotator cuff tearing. Most younger people who injure their rotator cuffs do so as a result of a traumatic injury such as a fall. Carpenters, mechanics, painters and others who do repetitive overhead activities have a greater chance of having rotator cuff issues. Tennis players, baseball pitchers, and other ball sports athletes are vulnerable to overuse partial thickness tears while participants of contact sports are at higher risk of acute tears.
Rotator Cuff Tear Symptoms:
The most common symptoms of a rotator cuff tear include:
- Recurrent pain with certain activities
- Pain that prevents sleeping on the injured side.
- A limited ability to move the arm, or weakness when lifting or rotating the arm.
- A crackling or “gritty” sensation when moving your shoulder.
A sudden tear will usually cause intense pain and may be associated with a snapping sensation and immediate weakness in your upper arm. A rotator cuff injury can make it painful to lift your arm out to the side.
Tears that occurs slowly over time due to overuse can also cause pain and arm weakness. You might have pain in your shoulder when doing overhead activities or when you reach for items. Over-the-counter medication, such as aspirin or ibuprofen, may relieve the pain at first.
Over time, the pain may become more noticeable at rest, and no longer goes away with medications. You may have pain when you lie on the painful side at night. The pain and weakness in the shoulder may make routine activities such as combing your hair or reaching behind your back more difficult.
Evaluation:
After a discussion of your general medical history, your doctor will ask you about your shoulder’s history including injury history, prior surgeries, duration of symptoms, disabilities related to your shoulder, location of pain, duration of pain, and aggravating and ameliorating activities. Additional information regarding previous treatments such as rest, activity modification, use of anti-inflammatory medications, and any physical therapy is helpful to the treating doctor.
A physical examination will be performed focusing on the following 5 general areas:
- Inspection – looking for muscle wasting, previous scars, or bony prominences
- Range of Motion – this will include assessment of both active (motion you perform) range of motion and passive (the doctor moves your arm) range of motion.
- Strength Testing – this will include isolated testing of each of the rotator cuff muscles by using tests such as the belly press test, lift-off test, Jobe test, Hornblower’s sign, and examining external rotation lag, Additional muscles such as the deltoid, biceps, triceps, and periscapular muscles will be tested as well.
- Provocative Tests – these tests will test for impingement, acromioclavicular joint arthritis, joint stability, and proper scapular motion.
- Neurologic and Vascular Assessment – this starts with range of motion of the neck and checks each nerve root that exits from the neck as well as checking for pulses at the wrist and normal blood flow throughout the limb.
Imaging Tests:
Other tests which may help your doctor confirm your diagnosis include:
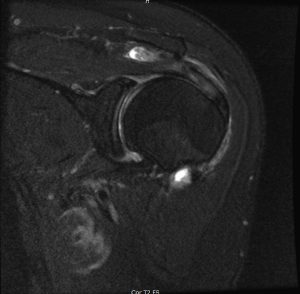
- X-rays. Xrays are utilized to show the bony architecture of the shoulder and the relationship of each individual to structure to one another. Additionally, they are helpful for showing arthritis in the joint or bone spurs. The limitations of xrays are it is a two-dimensional image of a three-dimensional structure and it does not adequately image soft tissue to evaluate the rotator cuff tendon.
- Magnetic resonance imaging (MRI) or ultrasound. These studies can better show soft tissues like the rotator cuff tendons. They can show the rotator cuff tear, as well as where the tear is located within the tendon and the size of the tear. An MRI can also give your doctor a better idea of how “old” or “new” a tear is because it can show the quality of the rotator cuff muscles. MRI also has the advantage of visualizing deeper structures in the shoulder joint such as cartilage, ligaments, and a specialized tissue called the labrum. Although an MRI is very good at diagnosing soft tissue injuries of the shoulder, it is not 100% accurate in diagnosing rotator cuff tears – especially with partial tears of the subscapularis.
Treatment:
Treatment depends upon the severity of the symptoms and the size of the rotator cuff tear. Additionally, the duration of rotator cuff tear can affect your doctors to perform a repair. For partial thickness tears, small full thickness tears, or large chronic tears nonoperative therapy such as rest, activity modification, anti-inflammatories, and physical therapy can improve pain and function.
It has been shown that rotator cuff tears can get larger over time. Early treatment can prevent your symptoms from worsening and prevent muscle degeneration. Once a muscles tendon is completely torn from the bone, that muscle no longer has any structure to maintain its normal resting length. If a muscle is allowed to remain retracted it will undergo degeneration with fat and scar tissue replacing the muscle fibers. Once this degeneration occurs, repair of the rotator cuff tendon may not be possible.
Nonsurgical Treatment
In approximately 50% of patients, nonsurgical treatment plans improve pain symptoms and improve shoulder function, however, strength does not usually improve without surgical intervention. Nonsurgical treatment may include any of the following:
- Rest and limiting overhead activities and activities that cause shoulder pain. You may be prescribed a sling to help keep your shoulder still.
- NSAIDS (ibuprofen or naproxen) may be prescribed to help reduce inflammation and swelling.
- Physical therapy and strengthening exercises may help to restore movement and strengthen the shoulder in general. Stretching and flexibility exercises can help relieve pain and increase your range of motion.
- Steroid injections may be used to provide localized rather than systemic anti-inflammatory medication. Medications such as triamcinolone (similar to cortisone) are helpful in reducing inflammation.
Surgical Treatment
Surgical treatment may be recommended by your doctor, especially if your pain does not improve with nonsurgical intervention. Continued pain is the main indication for surgery. Your doctor may also suggest surgery if you are very active or you use your arms for overhead work or sports. If you have a large tear (greater than 3cm, your symptoms have persisted for 6-12 months, you have significant weakness and loss of function in your shoulder, or you tear was caused by an acute injury, then surgery may be a good option for you.
Surgery is performed to re-attach the tendon of the rotator cuff to the head of the humerus. There are several options for re-attachment that will be discussed with you by your surgeon. The best approach should match your individual health needs.
Several options are available for repairing rotator cuff tears. The type of approach used depends on the surgeons experience with certain procedures, your specific anatomy and the quality of the tendon and bone tissue. Many surgical repairs can be done as an outpatient and do not require overnight hospitalization. Other shoulder problems may also be present in your shoulder and your surgeon may be able to take care of those problems at the same time as your rotator cuff repair.
The three most common techniques are traditional open repair, arthroscopic repair, and mini-open repair. In the end each technique has its own advantages and disadvantages. Each has the same goal of repairing the tendon and promoting healing. Each method has been rated the same as far as patient satisfaction, pain relief, and overall improvement in strength.
Arthroscopic Repair
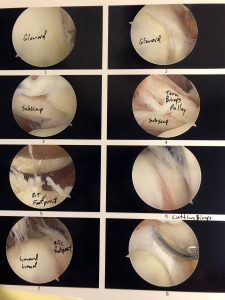

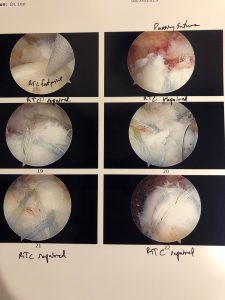
Arthroscopy is a procedure in which a small camera is inserted into your shoulder joint through four or five small incisions which are on average ½ of a centimeter in length. This allows the surgeon to approach your shoulder injury from the inside using tiny surgical instruments. This is a less invasive method for repairing defects in the shoulder. The postoperative pain may be less as well as healing time may be shortened through this approach in compared to other techniques.
Open Repair
A large or complex tear may require a traditional open approach. A larger incision is made over the shoulder and the deltoid muscle of the shoulder is detached to expose the torn tendon. At the same time an acromioplasty may be performed, this procedure is needed to remove bone spurs are removed from the underside of the acromion. A tendon transfer may also be required in order to increase the strength of the rotator cuff repair, often times this is more easily accomplished through a traditional approach.
During arthroscopy, your surgeon inserts the arthroscope and small instruments into your shoulder joint.
(Left) An arthroscopic view of a healthy shoulder joint. (Center) In this image of a rotator cuff tear, a large gap can be seen between the edge of the rotator cuff tendon and the humeral head. (Right) The tendon has been re-attached to the humeral head with sutures.
Mini-Open Repair
A mini-open repair uses a combination of arthroscopy and an open repair approach. Arthroscopy is used to evaluate shoulder and make any repairs within the joint, then the rotator cuff is repaired through a small incision on the shoulder. This avoids the need to detach the deltoid muscle and improves healing time.
Rehabilitation:
Rehabilitation is a key player in getting you back to your daily activities or participation in sports and recreational activities. A good physical therapy program will help you regain strength and range of motion. Therapy after surgery will progress in stages. Each patient is different and will progress through different stages at different times. Try not to be frustrated if you progress more slowly through your rehabilitation that others who have had rotator cuff surgery. Each patient, each injury, and each surgery is unique. Rehabilitation is a slow process and your commitment is key in having a successful outcome.
Immobilization
The repair the surgeon made in your rotator cuff tendon needs to be protected and allowed time to heal back down the bone. Often a sling is used to protect your shoulder for the first 4-6 weeks. The length of time in a sling will depend on the severity of your injury.
Passive Exercise
Your arm will remain weak even though the tendon has been repaired. At 4-6 weeks, or once it is safe to do so, your surgeon will have you start the process of regaining your range of motion through exercises and movements. Your therapist will help you with passive exercises to improve range of motion in your shoulder. The therapist will support your arm as it is moved through different positions.
Active Exercise
After several weeks of doing passive range of motion exercises, you will progress to moving your shoulder on your own through active range of motion exercises. This will allow your muscles to slowly start to regain the strength they have lost. At 8-12 weeks after surgery you will start a program to actively strengthen your shoulder muscles. At 4-6 months after surgery most patients have regained much of their range of motion and strength.
Outcome:
Each surgical technique has similar results in terms of pain relief and improved shoulder function. The comfort level of the surgeon with the patient’s preferred technique is important for an excellent outcome. Several factors may contribute to poor results following surgery. These include:
- Poor tendon quality
- Large tears and tears involving multiple rotator cuff tendons.
- Degeneration of the rotator cuff muscle – seen on MRI
- Poor patient compliance with restrictions and rehabilitation
- Patient age (older than 65 years)
- Smoking and use of other nicotine products
- Workers’ compensation claims
Complications:
Surgery in general carries a certain amount of risk such as blood loss or risks associated with anesthesia. A small percentage of patients may experience complications specific to rotator cuff surgery. Rotator cuff surgery complications may include:
- Injury to the nerve that regulates the use of your deltoid muscle.
- Infection. Patients are given antibiotics during the procedure to lessen the risk for infection. If an infection develops, an additional surgery or prolonged antibiotic treatment may be needed.
- Deltoid detachment. During an open repair, this shoulder muscle is detached to provide better access to the rotator cuff. It is stitched back into place at the end of the procedure. It is very important to protect this area after surgery and during rehabilitation to allow it to heal.
- Stiffness. Early rehabilitation lessens the likelihood of permanent stiffness or loss of motion. Most of the time, stiffness will improve with more aggressive therapy and exercise.
- Tendon re-tear. There is a chance for re-tear following all types of repairs. Repeat surgery is only indicated if there is severe pain or loss of function.
Phase I: Passive Range of Motion
Rotator Cuff Tear
This is the healing phase, the strength of the repair is limited to the strength of the sutures and bone anchors. At 4 weeks following surgery, the tendon repair has only approximately 20% of the strength of a native tendon. Because of this relative weakness and the risk of re-tear no active motion of the arm is permitted. Any active movement may pull on the repair and disrupt the tendon anchored to the bone.
Goals:
- Protect the tendon repair while gently gaining motion.
- Prevent the formation of adhesions and scar tissue.
- Reduce inflammation and pain
- Keep tension off of the repair through the use of a sling and abduction pillow.
Activities to avoid:
- No active range of motion. Do not move your arm yourself even if you have minimal pain or swelling.
- Do not push yourself up from a lying or seated position. This puts stress on the repair.
- Avoid aggressive stretching or passive range of motion that provokes muscle spasm.
What you should do:
- You may shower with your waterproof dressing 48 hours after surgery. You may let water run over your shoulder without dressings one week following surgery. No baths, no pools, and no soaking the wound until the skin is completely healed. While bathing, keep your forearm at your side against your hip bone to prevent internal rotation of your shoulder.
- You can do your normal everyday activities as long as you keep your arm in a sling. You may exercise sitting on a stationary bicycle while wearing your sling, no running at this point.
- Ice your shoulder regularly 3-4 times a day for up to 30 minutes at each session. You can use your Thermotek, Gameready, or an ice pack.
- Physical therapy should be initiated as soon as possible after surgery. Gentle range of motion, ultrasound, and gentle massage can help to decrease swelling and pain following surgery. The timing of physical therapy will be determined by the size of your tear, tissue quality of your rotator cuff, and whether or not you had other repairs in your shoulder.
- Your therapist will have you work on activities that enhance mobility of the joints in your shoulder, arm, and hand.
- When lying on your back keep a pillow or towel under your elbow to prevent extension of your shoulder. This will help reduce pain.
- Keep your arm in your sling/immobilizer. Move it only for bathing and for your prescribed exercises. Immobilization is typically up to 4 weeks and can be even longer depending on the extent of your injury. You will be gradually weaned from your sling in controlled environments.
- Light activities at waist level can be considered after week 6.
Therapy:
- You will do home shoulder exercises up to 3 times daily. You will be given guidance based on the extent of your injury and your level of pain.
- Physical therapy will be 1-3 times a week depending on your progression.
- Heat may be used prior to treatment and ice after treatment.
- Ice, heat, e-stim may be used to reduce pain and inflammation.
- Passive range of motion exercises will be performed with your therapist. Your shoulder muscles should be relaxed and not active during these motions. Family members may be taught how to assist you with passive range of motion at home.
- Supine passive elevation to 90 degrees.
- Sitting external rotation to 30 degrees.
- No internal rotation at this time.
- Initial exercises are performed while lying on your back to minimize gravity and ensure that your shoulder muscles are more relaxed.
- Pendulum hangs may begin, but you are not to actively move your arm.
- Shoulder blade pinches and rolls
- Passive range of motion for your elbow will begin if you had a biceps tendon tenodesis or tenotomy.
- Active range of motion of the elbow (non-weighted curls)
- Your hand and wrist need to be exercised (that is what the ball on your sling is for).
Goals for advancement:
- Appropriate healing of the tendon repair and other surgical repairs made during your surgery.
- Adherence to immobilization guidelines and precautions.
- Range of motion gained as determined by your surgeon and physical therapist. Typically 120-140 degrees of passive forward elevation and 30-60 degrees of passive external rotation with your arm at your side.
- Good control of pain and inflammation.
Phase II: Active Range of Motion (post-op week 6-12)
During this phase, your repair is still healing. After post-op week four, your repair is starting to have greater than 20% of the strength of a native tendon. This will allow you to do assisted active range of motion and progress to active range of motion. This is the stage in which you will start to normalize your motion and daily activities. After 8 weeks the tendon will be about 40% as strong as a native tendon, after 12 weeks it will be about 60% as strong.
Activities to avoid:
- No lifting objects heavier than a cup of water.
- No activities that are outside of your comfortable range of motion.
- Do not try to support your body weight by your hands or arms.
- Do not try to reach behind your back.
- Avoid any sudden jerking motions.
What you should do:
- Actively use your arm for bathing, dressing, driving, eating, drinking, using a computer.
- You may exercise using an elliptical machine, but do not support your body weight with your operated arm, no running.
- Continue to do your prescribed home exercises as instructed by your therapist. Your therapist will determine the frequency of your exercises based on your shoulder pain.
- Continue to go to your physical therapy appointments. These may be from 1-3 times a week depending on how you are progressing.
- You may use heat prior to therapy and ice after therapy.
- Local modalities may be used to help reduce your pain and inflammation in the physical therapy clinic.
- Supine passive range of motion with a pillow behind the elbow to prevent extension.
- Forward elevation: to tolerated
- External rotation at multiple angles to tolerated
- Scapular plane abduction to tolerated angle
- Assisted or pool therapy
- Stretch into flexion
- External rotation
- Active-assisted range of motion exercises usually start at 6 weeks post-op depending on the extent of your repairs and your progression.
- Elevation: lying on back, sitting, then standing
- External rotation: lying on back, sitting, then standing
- Pendulums mobility exercise
- Active range of motion starts at between 6 and 8 weeks postop based on your injury and progress.
- Forward elevation in the plane of the scapula
- External rotation, multiple positions and angles
- Once you have progressed to having good active range of motion, your therapist will establish a base strengthening program for your deltoid, scapula, and non-repaired segments of the rotator cuff. This typically occurs between 10-12 weeks post-op for small tears. Progression to this phase may take 16 or more weeks for large to massive rotator cuff tears.
- Resistance exercises
- Scapula strengthening
- Low level closed chain programs start
Achievements before progression to Phase III:
Adequate range of motion in all planes as determined by your MD and physical therapist.
Good shoulder blade positioning at rest and with activity.
Completion of phase II without pain or difficulty.
Minimal pain.
Phase III: Strengthening (postop weeks 12-16)
At this point in your rehabilitation, after 12 weeks the tendon is 60% as strong as normal, and after 16 weeks, the tendon is about 70% as strong as a normal tendon. At about 32 weeks after your operation the repair is about 80% as strong as a normal tendon. This allows you to start the initial strengthening phase of rehabilitation. You should have gained full range of motion by now and have good shoulder stability. By the end of this phase, you will return to normal functional activities and modified recreational activities.
Things to avoid:
- No jerking movements
- No sudden lifting or pushing
- No lifting heavier than 5 lbs
- No uncontrolled movements
- No straight arm raises out to your side
- No forward arm raises with your thumb pointed down. Always perform these with your thumb pointed up.
What you should do:
- Continue with your home exercises. You may be gradually weaned down to less and less often during this phase based on your progress.
- Visits to the physical therapy clinic will continue 1-2 times a week based on how your motion and strength is progressing.
- Heat prior to therapy, ice after therapy.
- Shoulder stretching may be more aggressive.
- Continue assisted or pool stretching.
- Progressive strengthening with increasing resistance.
- Begin lifting free weights (1-4 lbs)
- Exercises as determined by your physical therapist and surgeon based on your progression and extent of your injury.
Achievements before progressing to phase IV:
- Toleration of progression to functional activities
- Return of strength and shoulder stability so that you can progress to higher demanding work and sport specific activities.
Phase IV: Return to sports and recreation activities (Postop weeks 16-32)
This phase of rehabilitation will help you return to higher level functional activities such as sports, recreation, and work related activities. Your therapist will be instrumental in designing a program to help you continue to enhance functional use of your arm. You will continue stretching and working on range of motion during this phase.
Things to avoid:
- No lifting greater than 10 lbs
- No sudden lifting or pushing
- No progression into activities that are painful or you do not have adequate ROM and strength to do.
What you should be doing:
- Daily stretching
- Strengthening program at least 3 days a week.
- Progressive strengthening and endurance exercises. This may transition into general upper body strengthening with a progressive return to a weight lifting program.
- Transitioning into specific sports, work and hobbies.
Achievements for returning to full sport, work, and hobbies:
- Clearance from your surgeon and therapist
- No to minimal pain
- Full range of motion for full participation
- Adequate shoulder strength for desired activity
- Regular completion of strengthening program at least 3 days a week.